Racial and Ethnic Health Disparities and Addiction
Butler Center for Research - December 2022

Introduction
Download the Racial and Ethnic Health Disparities and Addiction Research Update
The United States has become increasingly diverse. According to the 2020 U.S. Census, approximately 42.2% of the population belongs to a racial or ethnic minority group while 57.8% of the population was White alone, non-Hispanic (a decrease from 63.7% in 2010).1 In order to meet the needs of the growing racial and ethnic minority populations, more attention is needed to address racial disparities in healthcare, particularly for addiction treatment.
The Centers for Disease Control and Prevention (CDC) defines health disparities as, "preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations."2 Healthy People 2020, the federal government's statement of national health objectives and prevention agenda, defines a health disparity as, "a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage" and notes that these disparities "adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; gender; age; mental health, cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion."3 The CDC defines racism as a system consisting of structures, policies, practices, and norms that assigns value and determines opportunity based on the way people look or the color of their skin, and which results in conditions that unfairly advantage some and disadvantage others, placing racial and ethnic minorities at greater risk for poor health outcomes.4
For members of racial and ethnic minority groups, significant health disparities persist. For example:
- In 2018, HIV deaths in Black populations remain more than 6 times as high as HIV deaths in White populations (6.2 deaths per 100,000 population vs. 0.9 deaths per 100,000 population).5
- Tuberculosis (TB) disproportionately affects some groups depending on various demographic, health, and social factors. In 2020, the majority of persons with TB disease in the United States identified as:6
- Asian persons; 35.8%
- Latinx persons; 29.7%
- Black persons; 19.6%
- White persons; 11.0%
- A 2019 study tracked diabetes rates among 7,575 adults between 2011–2016. The age and sex-adjusted prevalence of diabetes was as follows:7
- 22.1% for Latinx people
- 20.4% for Black people
- 19.1% for Asian people
- 12.1% for White people
Reducing disparities in health coverage, chronic health conditions, mental health, and mortality across racial and ethnic groups in the United States will require long-term efforts to address social determinants of health, such as poverty, segregation, environmental hazards, and racial discrimination.
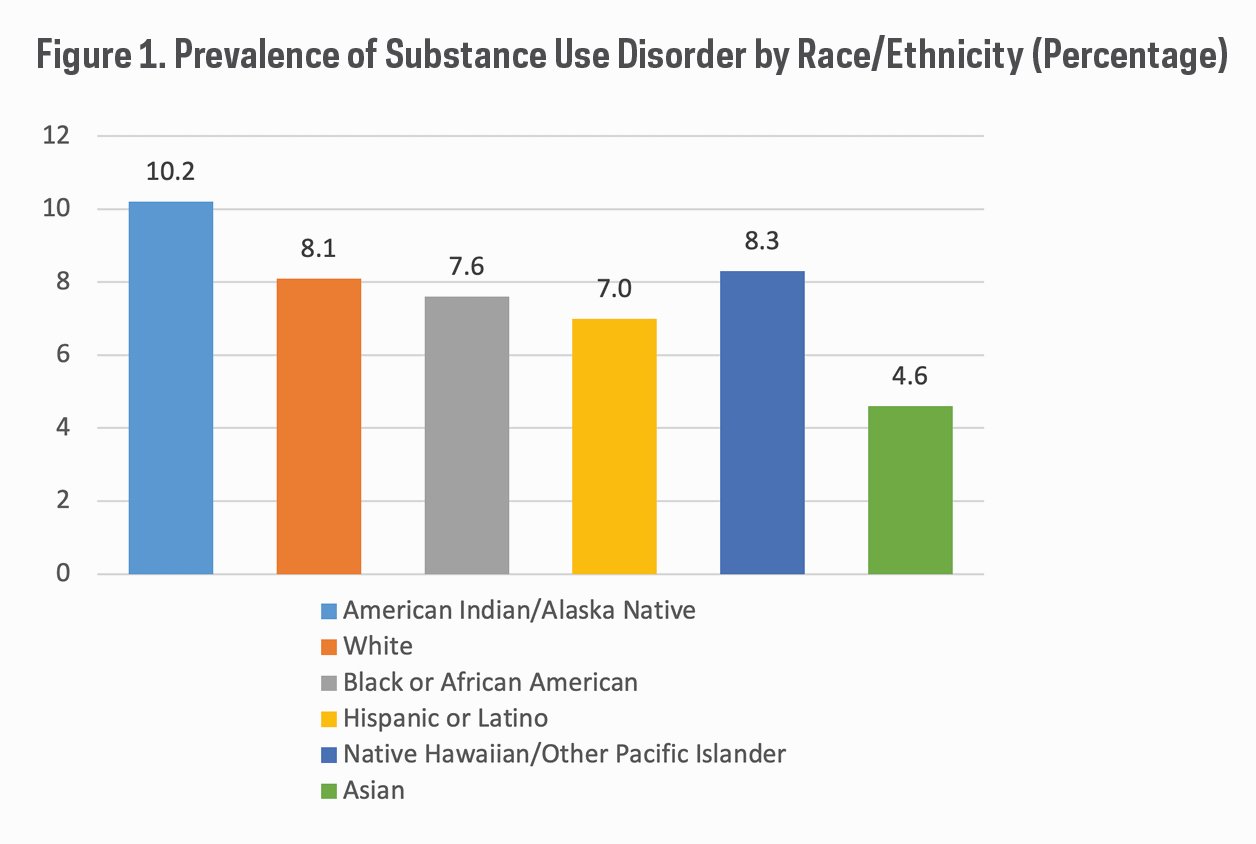
Figure 1 presents 2019 past-year substance use disorder (SUD) prevalence rates among those aged 12 and older by race and ethnicity, according to the Substance Abuse and Mental Health Services Administration (SAMHSA).8
Some racial and ethnic groups experience disparities in entering and receiving SUD treatment services. For example, an analysis of longitudinal data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) showed that individuals from most racial and ethnic groups were less likely to receive an alcohol intervention than were White individuals over a 3-year period.9
Lack of access to health coverage and SUD care is a problem among all racial and ethnic groups, but racial and ethnic minorities often face greater barriers to high-quality SUD treatment services. Black, Latinx, Native Hawaiian/Pacific Islander and nonelderly American Indian/Alaska Native people are more likely than White people to be uninsured, which can prevent access to quality SUD treatment.10
Opioid use disorder (OUD) and overdoses affect increasing numbers of Americans. Patients with OUD can be effectively helped with medication-assisted treatment. However, recent research has shown that racial and ethnic disparities exist in the prescribing of medications for OUD. For example, in a 2019 study that analyzed national survey data on clinic visits for OUD from 2004 to 2015, researchers focused on patients receiving prescriptions for buprenorphine, one of three drugs typically used to treat patients with opioid use disorder. After accounting for insurance status and other factors that can impact access to drug addiction treatment, Black patients were 77% less likely to receive buprenorphine prescriptions than White individuals.11 Additionally, a study of commercially insured people who suffered a nonfatal opioid overdose and were treated at an emergency room found that, compared with White patients, Black patients were half as likely to obtain follow-up treatment through filled prescriptions for buprenorphine or naltrexone, an encounter in the outpatient setting, or inpatient treatment and Latinx patients were also less likely to obtain follow-up treatment.12
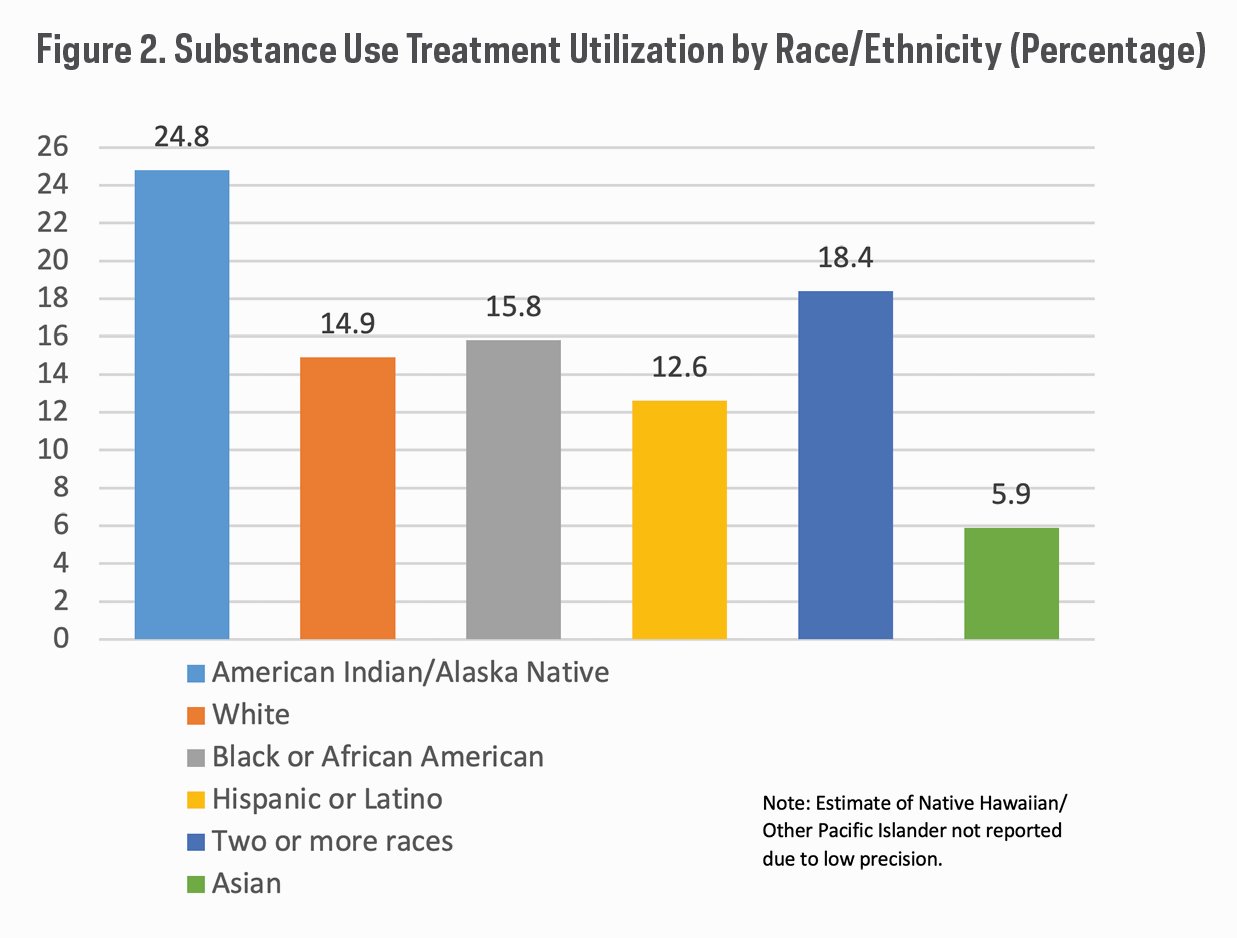
Racial and ethnic health disparities in substance use disorders remain a significant public health concern yet data reveal that treatment gaps continue to be significant. Figure 2 presents overall annual averages for the 2015 to 2019 National Surveys on Drug Use and Health (NSDUHs) for past year substance use treatment utilization at any location among people aged 12 or older who needed substance use treatment.13
When reviewing treatment admission rates for specialty SUD treatment (formal programs specifically designed to treat SUD such as rehabilitation, inpatient/outpatient services), racial and ethnic disparities exist. The racial and ethnic composition of admissions for specialty SUD treatment aged 12 years and older between 2009 and 2019 was as follows:14
- Admissions of White individuals increased from 65% in 2009 to 66% of all admissions in 2019.
- Admissions of Black individuals declined from 22% in 2009 to 20% of all admissions in 2019.
- Admissions of Latinx individuals comprised between 14% and 15% of all admissions in each year between 2009 and 2019.
Additionally, an analysis of combined data from the NSDUH survey for years 2015, 2016, and 2017 found that among those with SUD, Black individuals were 26% less likely and Latinx individuals were 29% less likely than their White counterparts to have used specialty SUD treatment in the past year.15
Several studies have shown that Latinx individuals especially underutilize specialty substance abuse treatment services: only 3–7% of Latinx individuals with substance abuse disorder report ever using specialty substance abuse treatment.16, 17, 18 Disparities in treatment utilization are especially pronounced between Latinx and White individuals.17, 18, 19
While available research is mixed, some studies find that racial and ethnic minorities who get treatment are more likely to report having negative experiences during treatment.20 This may be due to stigma, a lack of culturally responsive and respectful care, and a shortage of Black and Latinx clinicians.21, 22 Racial and ethnic minorities are also more likely to enter treatment later in their addiction process.23, 24
Ensuring that patients complete treatment is critical as it is associated with longer term abstinence, fewer relapses, fewer readmissions, higher levels of employment, less criminal involvement, and better overall health.25 However, not all racial and ethnic groups are equally as likely to complete treatment.21, 26 For example, using the Treatment Episode Dataset-Discharge (TEDS-D) dataset, a study analyzed treatment completion episodes and found that White participants had the highest completion rate (50%) while Latinx (47%) and Black participants were significantly lower (40%).27
What can be done to address racial and ethnic health inequities in addiction treatment?
At the community level, partnerships with local organizations and leaders are critical to increase trust and decrease stigma against SUD treatment. With community engagement and partnership, treatments can be developed that are culturally responsive.22, 23 Understanding where community members go for trusted information, such as barber shops, beauty salons, and churches, are critical for delivering prevention education and providing links to treatment.22 Collaborations with community experts across service sectors, including housing, employment, and health care, are necessary to establish and maintain support for recovery from addiction.23
Beyond the standard of care in treatment, individuals from racial and ethnic minority communities require treatment that is responsive to their cultural, behavioral health, and social needs in order to be effective. This is critical to minimize lapses in treatment and ensure the appropriate length of time in treatment.28 There are several examples of successful culturally responsive interventions. The Motivational Interviewing and Community Reinforcement Approach uses culturally tailored evidence-based treatments for American Indians and Alaskan Natives for SUD, with results showing improvements in percent days abstinent, SUD severity, and negative consequences from baseline to the 12-month follow-up.29 Another example is the Imani Breakthrough Recovery Program, a faith-based initiative designed to be culturally responsive and trauma-informed while assisting Black and Latinx communities with SUD, by using wellness coaches and groups held in the local church.30 Culturally adapted motivational interviewing that explicitly considers social stressors and cultural influences can help reduce heavy drinking and frequency of related negative consequences among Latinx, particularly those who are less acculturated or encounter higher levels of discrimination.31
At the institutional and organizational level, one goal would be to increase the number of staff trained to provide racial and ethnic minority populations with culturally responsive SUD care. There are training programs that serve as good examples of enhanced coursework in addiction psychiatry and culturally responsive care. REACH (Recognizing and Eliminating disparities in Addiction through Culturally informed Healthcare), a SAMHSA-funded program based at Yale, is a 1-year program for medical students, psychiatry residents/fellows, advanced practice registered nurses/nurse practitioner trainees, and physician assistant trainees who identify from an underrepresented group in medicine.32, 33 ACCESS (Achieving Culturally Competent and Equitable Substance Use Services), is a Boston University School of Medicine/Boston Medical Center Health Resources and Services Administration funded initiative for psychiatry and psychology trainees to treat individuals with co-occurring mental illness and SUDs at federally qualified health centers. Staff at these health centers also attend seminars by ACCESS trainees on working with diverse patient populations who have co-occurring mental illness and SUDs.34
Recommendations for future substance use research include the recruiting of racial and ethnic minorities, focusing research on treatment issues that disproportionately affect racial and ethnic minorities, increasing the number of underrepresented racial and ethnic treatment researchers, and including the expertise of racial and ethnic minority investigators in decision-making on funding for treatment research. The inclusion of racial and ethnic minorities will increase the likelihood that studies will generate knowledge about treatment outcomes for specific racial and ethnic groups.35
Conclusion
There is a growing realization among healthcare researchers, clinicians, and advocates that a focus on racial health disparities is a critical aspect of improving healthcare outcomes and that activities toward improvement must bring together many elements of the healthcare delivery system. An understanding of how race and ethnicity impact access to, and outcomes of, health services and substance use treatment can provide valuable insight to health policy experts and advocates. Transformative change is needed to provide equitable, quality care to an increasingly diverse population and to ensure equal treatment in the delivery of care in order to improve health outcomes and overall well-being.
The Hazelden Betty Ford Foundation Experience
While the Hazelden Betty Ford Foundation has many areas of strength, our seven-decades-old organization has much work to do to truly serve all who are affected by substance use disorders and to eliminate disparities in access to treatment. We have an obligation to ourselves, our communities, and our industry to lift up more voices and broaden our banner.
Our collective ability to meet the challenges of today and thrive in the future is directly connected to having a diverse workforce, an inclusive culture, a strong presence in diverse communities, and the provision of culturally responsive care. We are actively engaged in this work now and committed long-term to ensuring Hazelden Betty Ford honors, serves and advocates for people from diverse and underrepresented backgrounds.
If you have questions about diversity, equity and inclusion at the Hazelden Betty Ford Foundation, please reach out to us at DEI@HazeldenBettyFord.org.
References
- U.S. Census Bureau. (2021). 2020 U.S. population more racially and ethnically diverse than measured in 2010. census.gov/library/stories/2021/08/2020-united-states-population-more-racially-ethnically-diverse-than-2010.html
- Centers for Disease Control and Prevention. (2020). Health disparities.
cdc.gov/healthyyouth/disparities/index.htm#1 - U.S. Department of Health and Human Services. (2008). The secretary’s advisory committee on national health promotion and disease prevention objectives for 2020: Phase I report. healthypeople.gov/sites/default/files/PhaseI_0.pdf
- Centers for Disease Control and Prevention. (2021). Racism and health.
cdc.gov/healthequity/racism-disparities/index.html - Agency for Healthcare Research and Quality. (2021). National healthcare quality and disparities report. ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2021qdr.pdf
- Centers for Disease Control and Prevention. (2021). Trends in tuberculosis, 2020. cdc.gov/tb/publications/factsheets/statistics/TBTrends.htm
- Cheng, Y. J., Kanaya, A. M., Araneta, M. R. G., Saydah, S. H., Kahn, H. S., Gregg, E. W., Fujimoto, W. Y., & Imperatore, G. (2019). Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. JAMA, 322(24), 2389–2398. doi.org/10.1001/jama.2019.19365
- Substance Abuse and Mental Health Services Administration. 2019 NSDUH Detailed Tables. (2020). Tables 5.5A and 5.5B. samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetTabsSect5pe2019.htm
- Mulia, N., Tam, T. W., & Schmidt, L. A. (2014). Disparities in the use and quality of alcohol treatment services and some proposed solutions to narrow the gap. Psychiatric Services, 65(5), 626–633. doi.org/10.1176/appi.ps.201300188
- Artiga, S., Hill, L., Orgera, K., & Damico, A. (2021, July 16). Health coverage by race and ethnicity, 2010–2019. Kaiser Family Foundation.
kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by
-race-and-ethnicity - Lagisetty, P. A., Ross, R., Bohnert, A., Clay, M., & Maust, D. T. (2019). Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry, 76(9), 979–981. doi.org/10.1001/jamapsychiatry.2019.0876
- Kilaru, A. S., Xiong, A., Lowenstein, M., Meisel, Z. F., Perrone, J., Khatri, U., Mitra, N., & Delgado, M. K. (2020). Incidence of treatment for opioid use disorder following nonfatal overdose in commercially insured patients. JAMA Network Open, 3(5), e205852. doi.org/10.1001/jamanetworkopen.2020.5852
- Center for Behavioral Health Statistics and Quality. (2021). Racial/ethnic differences in substance use, substance use disorders, and substance use treatment utilization among people aged 12 or older (2015–2019). samhsa.gov/data/sites/default/files/reports/rpt35326/2021NSDUHSUChartbook102221B.pdf
- Substance Abuse and Mental Health Services Administration. (2021). Treatment Episode Data Set (TEDS): 2019. Admissions to and discharges from publicly funded substance use treatment. samhsa.gov/data/sites/default/files/reports/rpt35314/2019_TEDS_3-1-22.pdf
- Pinedo, M. (2019). A current re-examination of racial/ethnic disparities in the use of substance abuse treatment: Do disparities persist? Drug and Alcohol Dependence, 202, 162–167. doi.org/10.1016/j.drugalcdep.2019.05.017
- Guerrero, E. G., March, J. C., Khachikian, T., Amaro, H., & Vega, W. A. (2013). Disparities in Latino substance use, service use, and treatment: Implications for culturally and evidence-based interventions under health care reform. Drug and Alcohol Dependence, 133(3), 805–813.
doi.org/10.1016/j.drugalcdep.2013.07.027 - Creedon, T. B., & Lê Cook, B. (2016). Access to mental health care increased but not for substance use, while disparities remain. Health Affairs, 35(6), 1017–1021. doi.org/10.1377/hlthaff.2016.0098
- Pinedo, M., Zemore, S., & Rogers, S. (2018). Understanding barriers to specialty substance abuse treatment among Latinos. Journal of Substance Abuse Treatment, 94, 1–8. doi.org/10.1016/j.jsat.2018.08.004
- Mulvaney-Day, N., DeAngelo, D., Chen, C., Cook, B. L., & Alegría, M. (2012). Unmet need for treatment for substance use disorders across race and ethnicity. Drug and Alcohol Dependence, 125(Suppl 1), S44–S50.
doi.org/10.1016/j.drugalcdep.2012.05.005 - Matsuzaka, S., & Knapp, M. (2020). Anti-racism and substance use treatment: Addiction does not discriminate, but do we? Journal of Ethnicity in Substance Abuse, 19(4), 567–93. doi.org/10.1080/15332640.2018.1548323
- Substance Abuse and Mental Health Services Administration. (2020). The opioid crisis and the Black/African American population: An urgent issue. store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP20-05-02-001_508%20Final.pdf
- Substance Abuse and Mental Health Services Administration. (2020).
The opioid crisis and the Hispanic/Latino population: An urgent issue.
store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP20-05-02-002.pdf - Lewis, B., Hoffman, L., Garcia, C. C., & Nixon, S. J. (2018). Race and socioeconomic status in substance use progression and treatment entry. Journal of Ethnicity in Substance Abuse, 17(2), 150–166.
doi.org/10.1080/15332640.2017.1336959 - Montgomery, L. T., Burlew, A. K., Haeny, A. M., & Jones, C. A. (2020). A systematic scoping review of research on Black participants in the National Drug Abuse Treatment Clinical Trials Network. Psychology of Addictive Behaviors, 34(1), 117–127. doi.org/10.1037/adb0000483
- Brorson, H. H., Arnevik, E. A., Rand-Hendriksen, K., & Duckert, F. (2013). Drop-out from addiction treatment: A systematic review of risk factors. Clinical Psychology Review, 33(8), 1010–1024.
doi.org/10.1016/j.cpr.2013.07.007 - Saloner, B., & Lê Cook, B. (2013). Blacks and Hispanics are less likely than Whites to complete addiction treatment, largely due to socioeconomic factors. Health Affairs, 32(1), 135–45. doi.org/10.1377/hlthaff.2011.0983
- Mennis, J., & Stahler, G. J. (2016). Racial and ethnic disparities in outpatient substance use disorder treatment episode completion for different substances. Journal of Substance Abuse Treatment, 63, 25–33.
doi.org/10.1016/j.jsat.2015.12.007 - Jordan, A., Mathis, M. L., & Isom, J. (2020). Achieving mental health equity: Addictions. Psychiatric Clinics of North America, 43(3), 487–500.
doi.org/10.1016/j.psc.2020.05.007 - Venner, K. L., Serier, K., Sarafin, R., Greenfield, B. L., Hirchak, K., Smith, J. E., & Witkiewitz, K. (2020). Culturally tailored evidence-based substance use disorder treatments are efficacious with an American Indian Southwest tribe: An open-label pilot-feasibility randomized controlled trial. Addiction, 116(4), 949–960. doi.org/10.1111/add.15191
- Bellamy, C. D., Costa, M., Wyatt, J., Mathis, M., Sloan, A., Budge, M., Blackman, K., Ocasio, L., Reis, G., Guy, K., Anderson, R., Stewart Copes, M., & Jordan, A. (2021). A collaborative culturally-centered and community-driven faith-based opioid recovery initiative: The Imani Breakthrough project. Social Work in Mental Health, 19(6), 558–567.
doi.org/10.1080/15332985.2021.1930329 - Lee, C. S., Colby, S. M., Rohsenow, D. J., Martin, R., Rosales, R., McCallum, T. T., Falcon, L., Almeida, J., & Cortés, D. E. (2019). A randomized controlled trial of motivational interviewing tailored for heavy drinking Latinxs. Journal of Consulting and Clinical Psychology, 87(9), 815–830.
doi.org/10.1037/ccp0000428 - American Academy of Addiction Psychiatry. REACH. Recognizing and Eliminating disparities in Addiction through Culturally informed Healthcare. (n.d.). reachgrant.org
- Jordan, A., & Jegede, O. (2020). Building outreach and diversity in the field of addictions. The American Journal on Addictions, 29(5), 413–417.
doi.org/10.1111/ajad.13097 - Boston University School of Medicine/Boston Medical Center. Achieving Culturally Competent and Equitable Substance Use Services (ACCESS). cmmh-cmtp.org/pdfs/ACCESS-TrainingTrackPresentation06252020.pdf
- Burlew, K., McCuistian, C., & Szapocznik, J. (2021). Racial/ethnic equity in substance use treatment research: The way forward. Addiction Science & Clinical Practice, 16, 50. doi.org/10.1186/s13722-021-00256-4
